Epilepsy Monitoring Units (or EMUs) provide inpatients an evaluation of their seizures by top medical professionals using world-class technologies including around the clock EEG recording and synchronized video recording. Inpatients to an extended stay at an EMU often have refractory epilepsy, or seizures that cannot be controlled through medication. In my case, I was under evaluation to determine if I was a candidate for brain surgery.
As an inpatient, I’ve visited the same EMU twice. The first was for a nine-day stint, where unfortunately I did not exhibit any seizure activity. About half a year later, my second stay was for five days, during which I had three seizures including a secondary onset tonic-clonic seizure that the doctors tell me “went to eleven”.

Over my two stays, I certainly learned a lot about the inner workings of an EMU, how to prepare for a visit, and how to keep myself busy for days while connected via an electroencephalogram (or EEG) around the clock.
Goals While in the EMU
Your medical team’s goals are to create a safe, ideal situation to record the necessary data required to learn more about how your seizures originate and move through your brain. While your Neurologist will get access to the data feed, she is not the one that will watch you twenty-four hours a day during your stay. This means administrators that are monitoring you must recognize the seizure and mark the date/time to ensure that your neurologist gets the necessary data. To help them, it is your responsibility to help them understand the symptoms of your seizures. Of course, not all seizures are easily recognizable by medical professionals or the administrators watching the video feed. For example, during my second stay, an observant administrator explained that I had a focal seizure without even knowing it. The more the staff knows about your symptoms the easier it will be to tag the date and time so a Neurologist can look at the data later.
Remember, every few hours a new batch of nurses, administrators, and doctors will shift into the EMU. During their rounds, they will introduce themselves to you. As they do, be diligent to ensure that each understands the symptoms of your seizures. Don’t assume that all of the necessary information about you will shift to the next person.
Let’s talk about the goal of the patient. Your goal should be to have as many seizures as possible during your stay. If you are anything like me, that probably sounds scary. I mean you’ve probably spent a good deal of your life trying to prevent your seizures (especially in public). However, you should think that in the EMU “anything goes”.
In the hope to initiate a seizure while you are connected to EEG, your doctor will play with every possible Trigger. They’ll decrease the medication you’re taking, reduce the amount of your sleep, or suggest changes in diet. To help them, it is your responsibility to help your medical team understand your possible Triggers. For example, does stress cause your seizures? What about alcohol? Heat? Sleep Deprivation?
Preparations Before Your Stay
Before you enter the EMU you should be aware that each has its own rules and regulations. Make sure that you read those closely because they give information regarding visiting hours and great advice regarding what to bring, what to wear, and who to bring with you. Here is some other advice I learned that weren’t exactly included in that documentation.
My first piece of advice comes from the great producer, director, and actor Mel Brooks, “Hope for the Best, Expect the Worst”. Though your stay might be initially scheduled for just a few days, if you and your doctors can’t get the data required, your stay might be extended. Hopefully, you will have all the seizures the doctors need on the first day you enter the EMU. Most of us can handle three days sitting in a bed. Cripes, it might sound like a great stay-cation from one’s everyday life. But what about when your stay grows to more than a week?
At the EMU at which I stayed, each patient had their own room including an individual washing area and bathroom with a shower. While attached via the EEG you won’t have access to the shower, of course. Administrators will strictly enforce that you stay in your bed except when for bathroom breaks. There are a couple of reasons for this. First, your bed is the safest place for you to be. Based on the types of seizures you exhibit, you might have a risk of falling to the ground. Second, the cameras are focused on your bed. If you were to have a seizure important data might be lost if you were sitting at a different location. So you remain in bed all day, but what about at night?
Sleeping in any hospital is tough; the EMU is no different. There are a lot of potential irritations: the constant beeping, light from the hallway, nurse checks, a new mattress, and of course there is a bundle of wires each ending with an electrode glued to your scalp.
While most of the documentation provided by EMUs will tell you to bring a sleeping mask, I suggest that you actually sleep with your mask at home for a couple of weeks before your visit. A sleeping mask was a relatively new experience for me. I spent the first night just mucking with the straps to get comfortable.
In my opinion, earplugs are another required accessory, though I don’t think the expense of sound-canceling earphones is justified. As a side-sleeper, earplugs are another thing with which I really struggled. Getting used to earplugs at home before your visit is a must.
Most EMUs will tell you to bring button-up clothing in which to sleep. During my first stay, I did not heed that advice. I made sure to correct that mistake during my second stay. While the EEG is connected to your head, there is no way to get a T-shirt pulled over your head. I admit, in my youth, I’ve worn a T-shirt for three continuous days. I mean like many of you, I went to University. After five days though, I pleaded with my wife to smuggle in scissors to just cut the T-Shirt off. On the ninth morning, I wanted to tear that shirt off Hulk-Hogan-style. So absolutely bring your button-up pajama top.
In my opinion, another clothing requirement is thick socks and open-toe sandals. I know. I know. I wouldn’t be caught dead with socks and sandals out in the real world either, but in the EMU they are a must. I found the thick socks to be a great barrier to the cold hospital air at night. The sandals are useful because, in some cases, based on your particular types of seizures and the length of stay, the administrators might allow you to walk around.
Entering the EMU
Often even before you find your room, EEG sensors will be attached to your scalp to ensure that monitoring of your brain occurs. By the time you’ve been scheduled to the Unit, you’ve probably already had one (or even more) EEGs. Maybe an Ambulatory EEG was even given. If you are new to an EEG, applying and removing the sensors to your scalp is completely painless. Removing the sensors is a bit messy because the glue they use to attach to your scalp often sticks in your hair. It will come out after a few quick washes with a lot of conditioner.
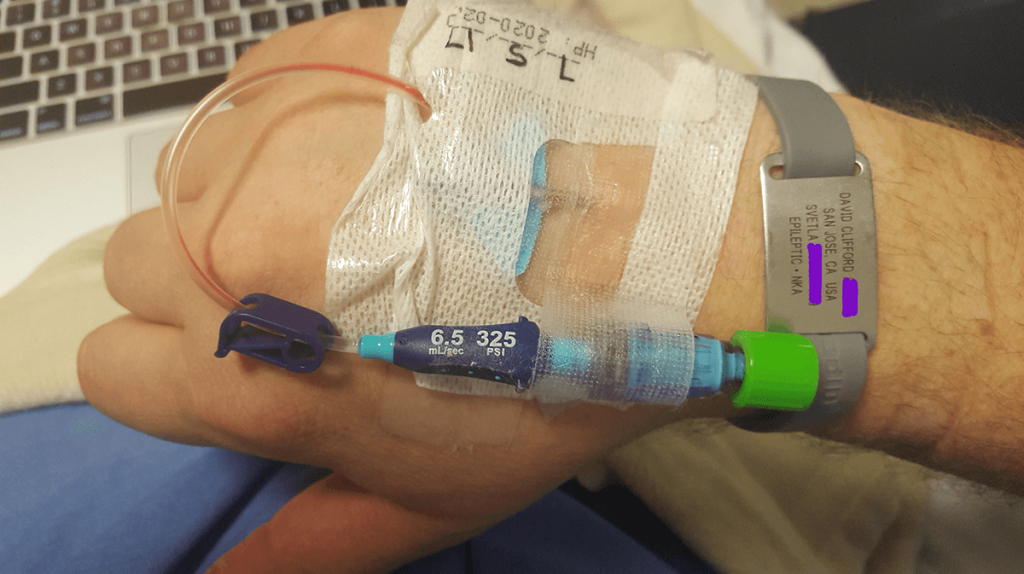
In your room, a nurse will apply a peripheral intravenous line for rescue medication. If you’re like me, you think that sounds pretty scary, but it shouldn’t. After a seizure occurs, the doctors will use this line to provide medication that will stop the seizure. After all, there is little information that they need after the seizure starts and allowing it to continue just increases the chances that something more sinister will happen.
After you are set up with your EEG, your bed, your rescue line, what do you do? You just wait.
Fighting the Boredom
Remember that long multi-state road trip you took with your family when you were a kid? Now, imagine it taking a week long. There’s just only so much one can do in the EMU before things get boring. There are things that you can do to prepare to keep yourself busy.
First, there is your smartphone. Preloaded with music and potentially video games. We’re all on them all the time anyway. It makes sense that you bring it and the charger with you. The EMU in which I stayed had free wifi so streaming wasn’t out of the question. If I were to enter a unit now, I would definitely take advantage of the download feature that some streaming services provide. I find watching videos on my phone strains my eyes, but it is definitely a solution.
The EMU in which I stayed had a television that included about eighty different titles streaming on demand. During the first stay, I must have watched the Guardians of the Galaxy at least twelve times. The second stay was mostly spent watching Captain America: Civil War. Live television was not provided so if your stay is scheduled during that big game or the highly anticipated season finale, make sure to schedule your DVR at home.
If you are a reader like me, I highly suggest bringing an eBook reader preloaded with a few books. If you can, I suggest that you bring an eBook reader that isn’t backlit as after just a few hours of reading my eyes quickly became quickly tired. Another piece of equipment I deem essential for any person like me that wears glasses is microfiber cleaning cloth. Remember, you can’t get up from the bed and bedsheets or button up pajamas make terrible cleaning equipment.
Leaving and After Your Stay
By the end of your stay, you and your medical team hopefully have got all of the necessary data about your seizures. If your medication was reduced to trigger the seizure, you probably will remain in the unit for an additional amount of time to ensure that the medication in your blood recovers back to levels to keep you safe.
The EMU at which I stayed wouldn’t release me unless I was in the care of someone else. That makes sense, of course. You ensure that there is someone there to get you home safely.
The first thing I wanted to do after both my stints? Run to my shower.
After the second stay, where I exhibited a few seizures, I also craved sleep. I know. It was counter-intuitive to me at the time as well. I just spent days in a bed and I wanted to go to sleep? I just wanted to go to sleep in my OWN bed. My point is that you shouldn’t assume that you are just going to jump back into your work routine the day after your visit to the unit.
Conclusion
An extended inpatient visit to the EMU can discover much-needed information regarding the class, origination, and severity of one’s seizures. Though the wait in the Unit can often seem unbearable, it isn’t as bad as not knowing the cause of one’s seizures. It was an incredibly valuable milestone for my care in my battle of Epilepsy. I highly suggest that anyone go through this process.
Do you have a visit planned as an inpatient to an EMU, we would love to answer any questions you might have.
For those of you that already have had an extended stay as an impatient in an EMU, did I miss anything? I would also love to hear any feedback, so we can make this article even better.
Meanwhile, join our community via Twitter at @BrazeAblaze. We would love to hear your story.
2 Comments
silicone bracelets PT · October 22, 2020 at 8:31 AM
Its good as your other posts :D, thank you for posting.
048: Jacked In - The Brain Ablaze Epilepsy Podcast · March 4, 2021 at 7:45 AM
[…] A stay at an Epilepsy Monitoring Unit can sound daunting. That’s why we wrote The Inpatient’s Definitive Guide to Epilepsy Monitoring Units. […]
Comments are closed.